With yoga, 'I felt my body change': Why so many are turning to complementary medicine
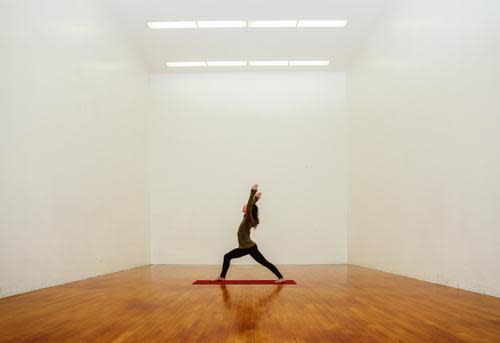
About one-third of Americans utilize some kind of complementary medicine approach — but is there science to back it all up? (Photo: Getty Images)
When I was diagnosed with fibromyalgia four years ago, my doctors prescribed a trifold regimen to treat my chronic pain: medication, cognitive-behavioral therapy, and exercise. Yoga, in particular, was the recommendation for my aching muscles and joints.
As someone used to popping a pain pill whenever symptoms arose, the idea of doing yoga as part of my treatment plan sounded, well, silly. But medication didn’t always work for my symptoms. Treatments for the condition — which is still considered new and mysterious, in the whole scheme of medicine — don’t work the same way for all people all the time.
Since I was unable to do high-impact exercise without provoking pain symptoms, I signed up for yoga. Slowly but surely, I felt my body change. Once tense and wracked with pain, the flows helped limber up my muscles and joints. The focus during my practice helped me get in touch with my body’s rapid-fire pain signals — but also ushered in a sense of control that fibro had once taken away. I could locate my pain early, and do something to change it.
I’m not alone in turning to something beyond a little orange bottle to manage my health— according to a new report from the Center for Disease Control and Prevention’s National Center for Health Statistics, roughly a third of the country utilizes some sort of complementary medicine approach. Complementary medicine is the use of alternative treatments to supplement a traditional approach, and includes mind-body practices such as yoga and tai chi, deep breathing, and meditation; non-vitamin/non-mineral dietary supplements like fish oil, probiotics, and glucosamine; acupuncture; chiropractic or osteopathic manipulation; and biofeedback.
A Growing Interest — And Demand
Overall, the use of complementary medicine has not significantly increased since 2002. However, specific treatment options have shown spikes, and doctors say their knowledge of — and patient demand for — alternative treatments is only growing.
“In my experience, the No. 1 prescriber of complementary medicine is the patient,” Michael Jonesco, DO, an internal medicine and sports medicine physician at The Ohio State University Wexner Medical Center, tells Yahoo Health. “They’re usually bringing in something the physician isn’t prescribing.”
But these practices aren’t just New Age, experimental forms of treatment. While some don’t have the same body of evidence to support their efficacy as other conventional practices, there is real science to support their use in certain cases.
“I’m a firm believer in evidence-based medicine, and there’s a big push right now to back practices up with numbers,” Jonesco says. “Some of the hard facts doctors have always accepted as givens are being challenged, and we need to be open to traditional and complementary forms of medicine.”
The evidence supporting complementary medicine is real and growing, says Houman Danesh, MD, director of Integrative Pain Management at Mount Sinai Hospital. “It’s no longer hokey,” he tells Yahoo Health. “There’s something like 27,000 medical articles on acupuncture alone, so its effects have been widely researched.”
Although it’s largely unknown why some techniques like acupuncture are effective, there are biological measurements that can be taken when an acupuncturist goes to work that show the body is responding. “You can actually measure the electroconductivity corresponding to the acupuncture points. So, what’s going on there?” says Danesh. “We’re not completely sure, but whatever the effects, I’ve definitely seen it work.”
He mentions one patient of his, a “poster child” of acupuncture’s effectiveness, who injured herself while cliff-diving. “While she had her pain symptoms under control, her life was in complete disarray,” Danesh explains. “She had a dependence on Percocet, and would count down the minutes every three hours between doses.” But after she started acupuncture for her pain, in three months, she was able to function normally again.
Supplements: Popular, But What’s The Science?
But acupuncture is one of the lesser-used practices in complementary medicine, according to the report. The most popular is something that’s gotten a lot more airtime in the media: supplement use. Roughly 18 percent of the U.S. adult population uses some sort of supplement to boost health.
As a sports medicine doctor, Jonesco says he frequently sees patients who ask about supplements. “If you’re not comfortable with this as a doctor, you’re missing out,” he says. “Patients want this.”
Related: 10 Sports Supplements That Actually Work
Particularly, he’s seen glucosamine help with joint pain, and says it’s probably the most common supplement he advises patients to use. “It’s probably the most studied in my field, and we’ve seen consistent improvements on it,” he explains. But like with any medical practice. It won’t work for everyone. “I usually say that if a patient wants to try it, we do a six- to eight-week regimen. If it works, great, continue. If not, save your money.”
Turmeric is also picking up steam in his office, something his doctor father has also used for years and turned him on to. “For instance, alternative specialists have looked into inflammatory arthritis in the U.S. versus India, where they don’t have the same prevalence,” Jonesco says. “Specifically, they looked at the diet and found that a key component that population was consuming, that U.S. adults were not, was turmeric.”
Jonesco regularly prescribes what he refers to as a “virgin bloody mary” to help his patients fighting injury or inflammation. “Basically, it’s a teaspoon of turmeric, a half teaspoon of black pepper, a half teaspoon of olive oil and about six ounces of V8 juice to help it go down smoother,” he explains. “The black pepper is meant to activate the turmeric, and the olive oil helps with absorption. I’ve seen a lot of success with this.”
Danesh agrees. Alternative, nutritionally based approaches won’t cure a person, but they won’t hurt — and can even help. “We think nothing of popping a couple Advil for pain and inflammation, but if it’s chronic, there can be side effects over time,” he says. “So why not, instead of the Advil, try eating foods that reduce inflammation in the body?”
Inflammation-fighting foods include healthy staples like berries, green tea, and salmon — which may explain why fish oil supplements are becoming more popular in the U.S., rising from 4.8 percent prevalence in 2007 to 7.8 in 2012. Fish oil provides a shot of omega-3 fatty acids, which have been shown to reduce inflammation.
If you’re still a skeptic, that’s fine, says Danesh. But don’t brush off a doctor who suggests a complementary approach, and don’t hesitate to mention an alternative treatment yourself. “I definitely have a lot of patients these days who come in and say, ‘I don’t want to put anything in my body,’ so we employ the alternative route,” he says. “But I also have people who come in and say, ‘I don’t really believe this stuff, but could it still work? Is it worth my time?’ And I always tell them that they don’t need to believe this for it to work.”
Yoga ‘Doesn’t Just Work For Mindfulness’
A prime example: Yoga — a practice that the National Center for Health Statistics report notes has seen a spike in recent years. The practices of yoga, tai chi, and qi gong have increased from 5.8 percent in the population in 2002 to 10.1 percent in 2012, with yoga being the most popular practice.
Recent research from the European Journal of Preventive Cardiology suggests yoga might be as effective as cardio exercise in terms of providing protective cardio benefits, in addition to reducing types of chronic pain.
Related: Yoga May Benefit Heart Health As Much As Aerobics
“It doesn’t just work for mindfulness,” says Danesh. “We are mostly seated in desks, flexing our hips. Yoga forces you to use muscles in ways you’re not necessarily used to with daily activity, providing flexibility and strength.”
I experienced this benefit when I began my yoga practice (and I, like many others, was a skeptic going into it). My muscle tone, which had withered away due to lack of movement from debilitating bouts of pain, slowly began rebuild. My body went from small and stiff, to lithe and lean. I felt mentally fresh every day, instead of foggy. I slept better at night.
And science seems to support this: a 2010 study from the journal Pain showed a host of major fibro symptoms lessened with yoga, including pain, fatigue, stiffness, sleep difficulties, depression, memory problems, anxiety, and poor balance.
In reporting their findings, the researchers wrote that “these improvements were shown to be not only statistically but also clinically significant, meaning the changes were large enough to have a practical impact on daily functioning.” Yogis in the study saw a 24 percent reduction in everyday pain compared with non-practitioners, while fatigue dropped by 30 percent and depression by 42 percent.
Deep Breathing And The Body-Brain Feedback Loop
But yoga isn’t the only thing that can help people experiencing a chronic pain condition: Deep breathing — the second most popular complementary health practice that’s used by 11 percent of adults in the U.S. — also seems to pass scientific muster.
“You have the power to consciously activate that parasympathetic nervous system, which will calm you down,” Diane Robinson, PhD, a neuropsychologist at UF Health Cancer Center - Orlando Health, tells Yahoo Health. “People always say, ‘Just breathe.’ It’s actually really true. Something as simple as slowing down your breath is a really sound physiological strategy.”
Here’s how it works: There’s a feedback loop from body to brain, and when you’re stressed, your brain is reading your body’s signals. If you allow your anxiety to control your thoughts, you’ll signal there’s a threat and your body will remain wired. But if you employ strategies of zen, you’re telling your body everything is fine.
“If you’re dealing with stress and you break that pattern, you are sending a message to your brain that you are OK, slowing down that release of chemicals,” Robinson says. “You’re actually sending yourself neurological messages to calm down.”
Alternative Medicine: Not One-Size-Fits-All
Jonesco says that complementary medicine is still working its way into the mainstream. “Some physicians tend to shove it off a bit … [saying], ‘that’s not what I learned.’ But more people want this, and we don’t want to see a disconnect between doctor and patient,” he says.
Just like traditional treatments such as medication or surgery, all forms of complementary medicine are not right for every person. But knowing options exist will increase the odds of effectively tackling all sorts of conditions. Look for a doctor who’s open, especially if you’re dealing with a condition that’s hard to treat.
“There’s a certain arc to medicine, but you have to have the best physical and mental approach to identify the right treatment for each patient,” Jonesco says. “Not every patient is a textbook case.”

